Healthcare has become undeniably unaffordable for companies, employees & their families.
This is how you take back control.
Build a Bespoke Health Plan
Easily transition for immediate & long-term savings. Mirror the plans you have today, access turn-key solutions & implement the right stop-loss, pharmacy strategy & $0 cost care options.
Build a Bespoke Health Plan
Easily transition for immediate & long-term savings. Mirror the plans you have today, access turn-key solutions & implement the right stop-loss, pharmacy strategy & $0 cost care options.
Deliver a New Service Model
A hospitality-style service model is people-centric.
We focus on the member first - guiding employees through the healthcare system with personal advocates for access to the right providers, fair pricing
& quality care.
Deliver a New Service Model
A hospitality-style service model is people-centric.
We focus on the member first - guiding employees through the healthcare system with personal advocates for access to the right providers, fair pricing
& quality care.
Manage & Control Claims Costs
Gain visibility to control the cost of the claim before it is paid. Lower plans & favorably impact stop-loss costs with proactive claims management.
Manage & Control Claims Costs
Gain visibility to control the cost of the claim before it is paid. Lower plans & favorably impact stop-loss costs with proactive claims management.
Gain Actionable Data
Make informed decisions with access to vetted solutions. Choose the right strategy with plan performance reviews, data visibility & real-time management.
Gain Actionable Data
Make informed decisions with access to vetted solutions. Choose the right strategy with plan performance reviews, data visibility & real-time management.
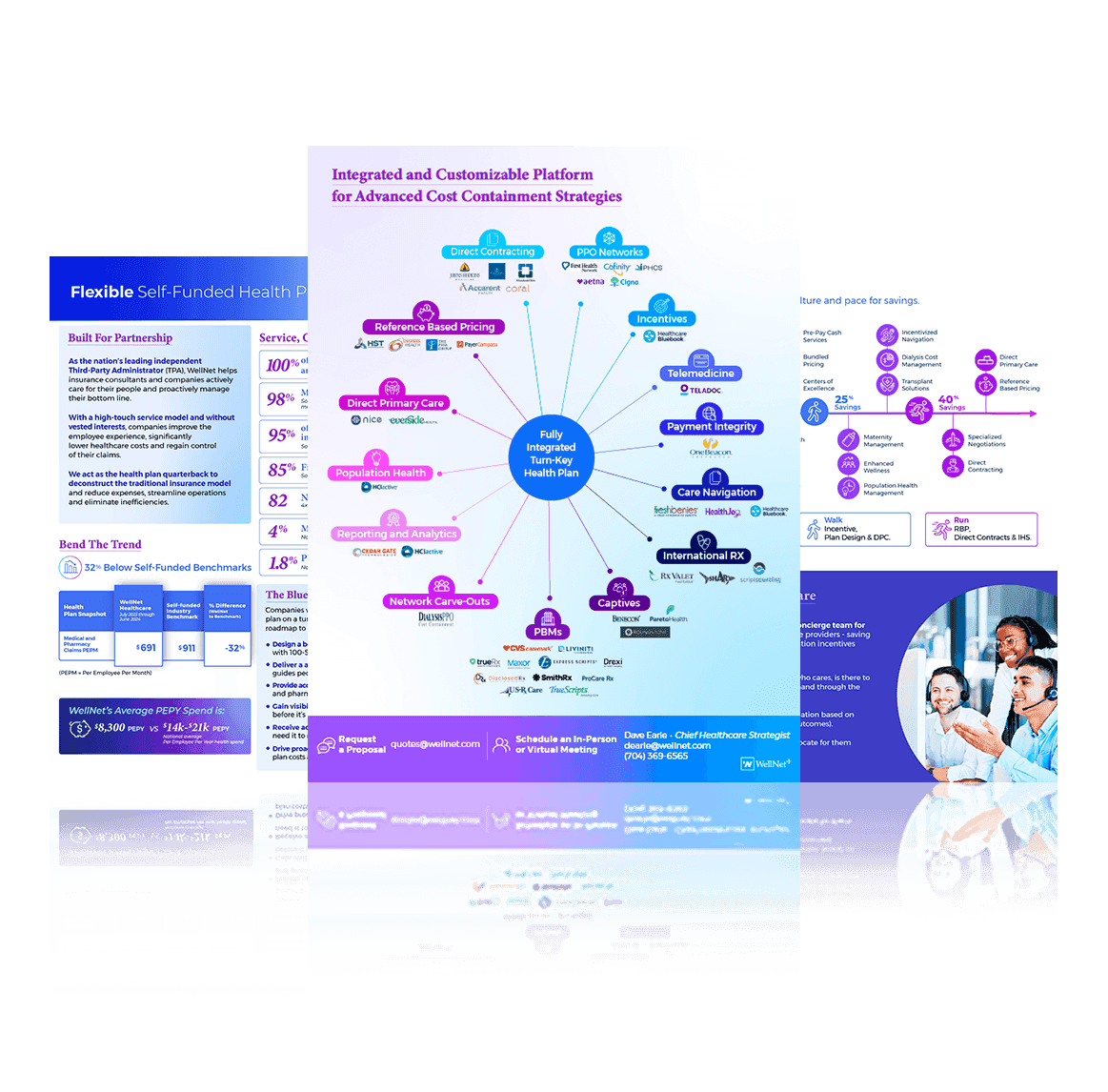
Go At
Your Own Pace
Custom plans use a 20+ point toolkit to fix, repair & upgrade your health plan. We call it Crawl, Walk, Run - knowing each company has its own pace, unique culture & blueprint for savings.
Go At
Your Own Pace
Custom plans use a 20+ point toolkit to fix, repair & upgrade your health plan. We call it Crawl, Walk, Run - knowing each company has its own pace, unique culture & blueprint for savings.
Significantly Improve Outcomes
Employees utilize a healthcare concierge team for guidance - saving companies 10% with care navigation incentives & creative plan designs.
Significantly Improve Outcomes
Employees utilize a healthcare concierge team for guidance - saving companies 10% with care navigation incentives & creative plan designs.
How Companies Bend The Trend
How Companies Bend The Trend
Download the quick-hit guide to rebuild health plans that improve the employee experience, significantly lower healthcare costs & reduce high-cost claims.
Explore WellNet
Actively care for your people.
Proactively manage the bottom line.
One Solution.
Integrated & customized for advanced cost containment strategies.
One Solution.
Integrated & customized for advanced cost containment strategies.

WellNet+
- Level-Funded & Self-Funded Health Plans
- Steerage Incentives
- Billing Errors
- International Rx Sourcing
- Medicare Eligible
- Pre-Pay Cash Services
- Advanced Imaging Carve-Out
- Dialysis Carve-Out PPO
- Direct Primary Care
- Direct Contracting
WellNet+

My Advocacy
- Expertly Trained Personal Advocates
- Real-Time Support & Ongoing Assistance
- Access to Quality Care & Free Resources
- Direct Savings on High-Cost Speciality Drugs & Procedures
- Manage Claims, Billing & Scheduling
My Advocacy

Blade
- Toolkit Analysis
- 20+ Performance Optimizers
- Enhance Plan Design
- Drive Down Claims Costs
- Proactive Pharmacy Management
Blade

Service, Outcomes
& Savings
Service, Outcomes
& Savings
Your on-demand resource center for all the best content - all in one place.
Start here for the best of WellNet content.
Come back for the latest & greatest.
“Control & transparency offered by WellNet are important in creating issue resolution and proactive cost management.”
Carlos Castresana -USI Insurance Services

The New Power Half-Hour
The New Power Half-Hour
Schedule a brief huddle to quickly learn more about how WellNet health plans save money & improve outcomes.
Like what you hear? Keep the convo going with a deep dive at your convenience.
Schedule a brief huddle to quickly learn more about how WellNet health plans save money & improve outcomes.
Like what you hear? Keep the convo going with a deep dive at your convenience.
Crawl, Walk, Run
Tailored for your unique culture
& pace for savings

Supercharge Your Outcomes
Supercharge Your Outcomes
Inside: 20+ ways our performance optimizers control the cost of the claim – before it’s paid.

Ask Us
Anything
Ask Us
Anything
If you’re interested in learning about WellNet solutions, reducing pharmacy costs, improving member advocacy, or simply want to dive deeper into self-funding education, we’re here to help.